Treating LDL-C alone doesn’t close the case on risk1,2
Lowering LDL-C sooner and longer improves outcomes4,5
Lower is good.
Earlier is even better.
Lower LDL early and keep it low. Sustained LDL-C lowering may delay ASCVD events by decades.4
25% Lower Lifetime LDL-C*
of ASCVD events4
50% Lower Lifetime LDL-C*
of ASCVD events4
*Individuals with average LDL-C levels
Even slight delays in managing LDL-C following an ASCVD event can lead to adverse outcomes7,8
There is no level of LDL-C that is considered “too low.”9
ASCVD events could be significantly reduced if more patients achieved evidence-based LDL-C goals10,11
Adding potent lipid-lowering therapy (LLT) to statins+ezetimibe in high-risk patients with elevated LDL-C could prevent10
≈ 8000
per 1 million treated patients
Nearly all these events would be nonfatal events, including MI, stroke, and revascularization, each associated with increased risk of future events
If all secondary prevention patients could be maintained at an LDL-C <70 mg/dL, it could prevent11
≈ 634,000
550,000 CHD events
198,000 ischemic strokes
244,000 CV deaths
22.5% of all ASCVD events could be averted
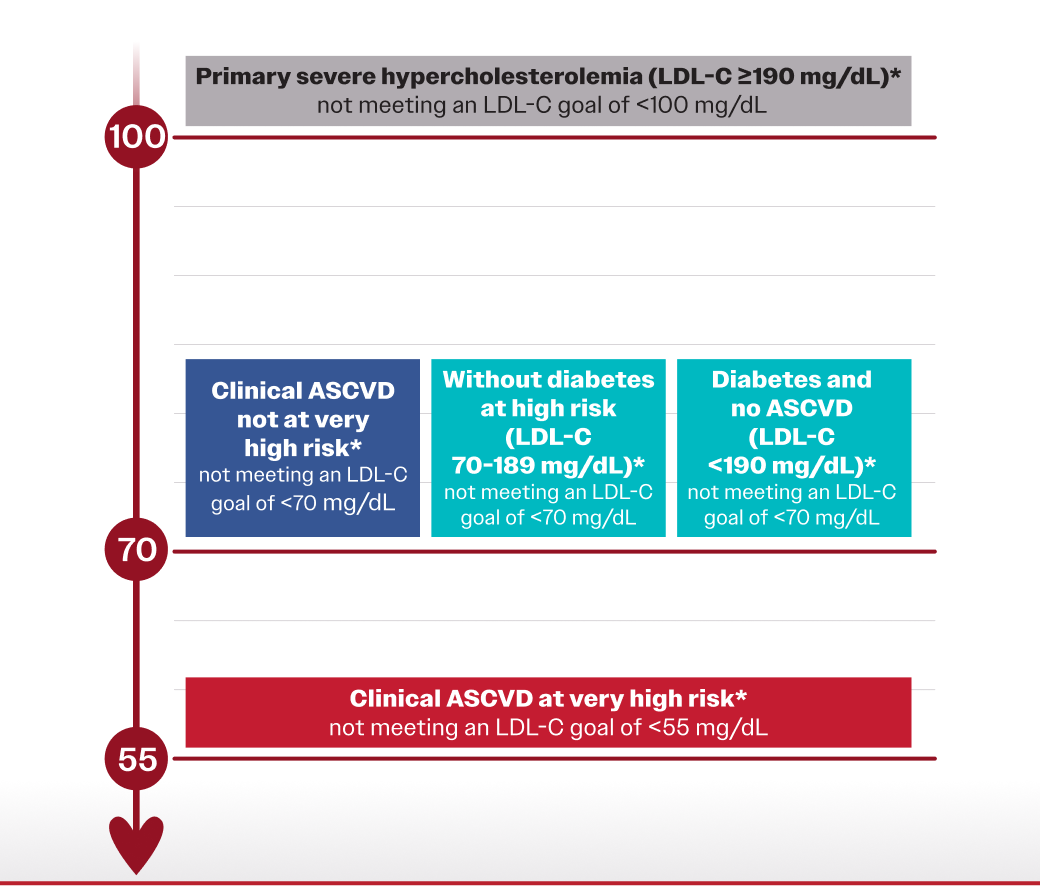
American College of Cardiology (ACC) 2022 expert recommendations
LDL-C thresholds9,*
<100mg/dL
<70mg/dL
<55mg/dL
*≥50% LDL-C reduction from baseline also considered a threshold for intensifying therapy.9
See the latest 2022 ACC guidance on nonstatin LDL-C therapies
Consider nonstatins when LDL-C remains elevated despite statin therapy9
*≥50% LDL-C reduction on maximally tolerated statin therapy.9
See how lipid factors contribute to ASCVD risk: LDL-C and beyond
References: 1. Matsuura Y, Kanter JE, Bornfeldt KE. Highlighting residual atherosclerotic cardiovascular disease risk. Arterioscler Thromb Vasc Biol. 2019;39(1):e1-e9. doi:10.1161/ATVBAHA.118.311999 2. Reijnders E, van der Laarse A, Jukema JW, Cobbaert CM. High residual cardiovascular risk after lipid-lowering: prime time for predictive, preventive, personalized, participatory, and psycho-cognitive medicine. Front Cardiovasc Med. 2023;10:1264319. doi:10.3389/fcvm.2023.1264319 3. Raja V, Aguiar C, Alsayed N, et al. Non-HDL-cholesterol in dyslipidemia: review of the state-of-the-art literature and outlook. Atherosclerosis. 2023;383:117312. doi:10.1016/j.atherosclerosis.2023.117312 4. Ference BA, Ginsberg HN, Graham I, et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. Eur Heart J. 2017;38(32):2459-2472. doi:10.1093/eurheartj/ehx144 5. Ray KK, Ference BA, Séverin T, et al. World Heart Federation Cholesterol Roadmap 2022. Glob Heart. 2022;17(1):75. doi:10.5334/gh.1154 6. Baigent C, Blackwell L, Emberson J, et al; Cholesterol Treatment Trialists’ (CTT) Collaboration. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376(9753):1670-1681. doi:10.1016/S0140-6736(10)61350-5 7. Kytö V, Saraste A, Tornio A. Early statin use and cardiovascular outcomes after myocardial infarction: a population-based case-control study. Atherosclerosis. 2022;354:8-14. doi:10.1016/j.atherosclerosis.2022.06.1019 8. Åivo J, Ruuskanen JO, Tornio A, Rautava P, Kytö V. Lack of statin therapy and outcomes after ischemic stroke: a population-based study. Stroke. 2023;54(3):781-790. doi:10.1161/STROKEAHA.122.040536 9. Lloyd-Jones DM, Morris PB, Ballantyne CM, et al. 2022 ACC expert consensus decision pathway on the role of nonstatin therapies for LDL-cholesterol lowering in the management of atherosclerotic cardiovascular disease risk: a report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2022;80(14):1366-1418. doi:10.1016/j.jacc.2022.07.006 10. Katzmann JL, Becker C, Bilitou A, Laufs U. Simulation study on LDL cholesterol target attainment, treatment costs, and ASCVD events with bempedoic acid in patients at high and very-high cardiovascular risk. PLoS One. 2022;17(10):e0276898. doi:10.1371/journal.pone.0276898 11. McKinley EC, Bittner VA, Brown TM, et al. The projected impact of population-wide achievement of LDL cholesterol <70 mg/dL on the number of recurrent events among US adults with ASCVD. Cardiovasc Drugs Ther. 2023;37(1):107-116. doi: 10.1007/s10557-021-07268-x